Brain-computer interfaces place electrodes right next to certain brain areas, reading electrical activity to convert specific thoughts and intentions into signals that can be used to control computers, mobile devices, and theoretically other things like electric wheelchairs and prosthetic limbs.
Initially, they'll chiefly be sold as medical devices that can bring communication, interaction, independence and a sense of humanity back to people who have lost motor functions as a result of spinal injuries, motor neuron disease and other afflictions. But others are looking forward to a future when they'll be implanted to augment healthy patients with new mind-controlled abilities.
Neuralink, Blackrock Neurotech, BrainGate and numerous other companies are making progress with brain-reading implants that place up to and over a thousand electrodes directly into the brain tissue for high-bandwidth and potentially two-way communications.
But to do so, they need to cut a hole in a patient's skull. That kind of thing can lead to all sorts of complications, both medical and regulatory, and frankly, people need a hole in the head about as much as ... well, something they don't need very much. Somebody should come up with an analogy for that.
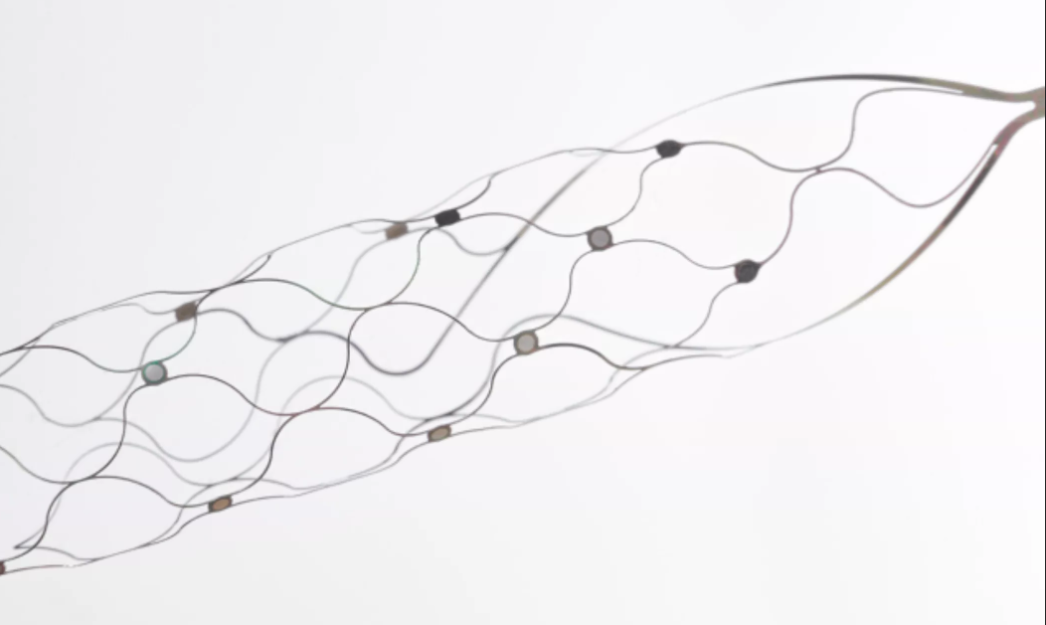
Synchron takes a different, and highly practical approach – this company has developed a "Stentrode" that can be implanted through the jugular vein, and steered through the brain's blood vessels to a position right next to the motor cortex. Here, it's deployed like a regular self-expanding stent, and it places 16 electrodes right next to specific brain areas that can be used to control devices wirelessly and instantly.
It's somewhat of a lo-fi approach compared to the thousand-electrode chips of Neuralink and other competitors – but Synchron co-founder and CTO Professor Nicholas Opie tells us that's actually a considerable advantage in these early days; the 10 human patients already fitted with a Stentrode are finding it incredibly reliable, they're learning to use it the day it's fitted, and they're finding it never needs re-calibration.
14 June 2018
The fact that any clinic can implant the device, plus the fact that the entire device is fully implanted, with nothing sticking through the skin, should make this a much simpler device for bodies like the FDA to approve, making for a potentially much quicker path to market that Synchron hopes will make the Stentrode widely available to disabled patients before the competition.
With some US$145 million in funding, notably including both the Gates Frontier and Bezos Expeditions organizations, Synchron is working toward pivotal trials to have the device approved for medical use.
We sat down for an extended chat with Professor Opie at Synchron's Australian office. What follows is an edited transcript of what he told us.
On Synchron's minimally-invasive brain-computer interface
Prof. Nicholas Opie: We're trying to create a world where people with paralysis are unencumbered by their disease. We want to be able to help these people communicate again, and in the long term, to be mobile and live independent lives.
There's decades of work showing that yes, you can record signals from the brain's motor cortex when people are thinking about performing actions, and translate them into commands that can be used by external equipment like computers or or wheelchairs.
The problem with the technology that's there at the moment is that it's all research – the FDA has not approved the use of these invasive devices. These technologies require open-brain surgery to access the brain and then putting electrodes directly onto the brain or penetrating into the delicate tissue itself.
There are a bunch of different layers over the brain – not least the skull – that attenuate and block electrical signals. So the best way to avoid them is to get under the skull. One way is by drilling or sawing and removing chunks of skull. We came up with a another way of getting there using blood vessels to to get underneath the skull, but in a way that doesn't require this invasive surgery.

Adam Glanzman/Synchron
On how the device is implanted
We gain access through the jugular vein, and then use the natural highways of the body to get to the motor cortex, just through blood vessels. When we're there, we deposit the Stentrode, a self-expanding nitinol stent implant with 16 electrodes distributed around it.
The vascular system is pretty well-mapped. Doctors already use similar procedures if you've got a blockage or a ruptured vessel or something like that. There's a long history of putting stents in blood vessels to keep them open. So our idea was: how about we use this as the method of getting in close contact with key brain regions, and create a brain/computer interface that's fully compatible with the infrastructure and equipment and skills that surgeons already have.
There are stroke centers everywhere, there's more of them popping up all the time. We've got mobile stroke centers now in Australia, and in other parts of the globe. So everything that's needed to implant this, including the skills of physicians, already exists. Some of the other technologies will need to build their own hospitals to do these procedures; were just taking advantage of what's already there. It's an in-and-out day procedure, no overnight stays or monitoring.
We use the same sort of self-expanding materials as a stent, but we use it as a scaffold on which to embed electrodes. We've got it down to a very small tube, you can use conventional catheter systems to get to the brain. When the catheter's removed, it expands and pushes the electrodes against the blood vessel wall.
Stentrode brain computer interface online in first two human patients
The blood vessel at the superior sagittal sinus, where we place our Stentrodes, is one of the main drainage channels for the brain. The diameter in that vessel is quite large – 4 to 7 mm. Our lead is quite tiny in comparison to some of the thick and chunky ones they use for pacing leads and other things.
The brain is pretty well organized. Each of the electrodes are designed to sit over a different part of the brain. And the accuracy we're seeing from clinicians is amazing. We originally asked them to get it within about 2 mm, but we see them getting it within half a millimeter all the time – that's more or less the resolution of the scanning equipment they've got, so they're very, very good.
Once that's deployed, the other end of the wire is plugged into a pacemaker-style device, you might say, that's sits under the skin in the chest. So the entire device is completely implanted.
On the advantages of using a stent as opposed to brain-penetrating electrodes
One of the issues with the other technologies is that they have exposed parts, wires and cables and things coming out of the brain. Big infection risk, obviously, so none of the patients that have those systems are able to use them at home. They can only use them when they come into a into a laboratory or clinical setting.
Removing and replacing parts of the skull ... well, some companies have done that with some success. There are some success stories where that's been fine. There are other horrifying stories where removing part of the skull and putting a metal implant in there is ... not ideal.
The brain really doesn't like having things stuffed in it. It's like a splinter, your body will try to reject it and push it out. Long before Neuralink, there's decades of work done by many groups with penetrating electrodes, and they're all facing that same problem.
For us, the blood vessel still wants to reject our device – but it rejects it by pushing it into the wall – and eventually covering it over with skin within a few weeks. That works in our favor, because it sort of pushes it closer to the brain, and anchors it in the wall. So we're using the body's responses to our advantage, and it doesn't impede the blood flow.
Synchron
On whether 16 electrodes is enough, given that other groups are looking at thousands
Sixteen electrodes is not a lot, compared to some of the other ones. The question is, what are you going to do with it? A lot of the patients we have at the moment, even though we've got 16, they only want to use one. They want to use it really reliably, safely, easily, without any calibration. They want it to work every time. That's enough for them to communicate, to use phones, use email, do shopping, online banking, all that stuff.
It depends on the program and what you're trying to do, but with one switch, or button, in conjunction with eye tracking, which some people can use, they can navigate around a screen and make a mouse click. As soon as you've got that, you can do more or less anything on a computer or a smartphone. You can control a smart home, the lights, the TV, that sort of thing.
If you bring in some more switches, it's not unreasonable to expect you might be able to control an electric wheelchair; forward, backward, left, right. Or similarly, to control a mouse pointer if you don't have the ability to use eye tracking. If you have 10 switches, maybe then you can do every finger, and perhaps you can use a keyboard much faster.
When you get to the number of switches some of the other groups are using, I suspect it goes beyond what a patient is actually going to be able to control. I mean, there's 88 keys and three pedals on a grand piano, but you're not talking about thousands. People don't control thousands of switches at a time.
Once you get to that kind of number, it goes beyond people intentionally trying to control switches, you start having to pick up subconscious signals and infer what needs to be done. We're going for the other side, we want people to control what they're doing, make a click exactly when and where they want it.
I think there'll be a time when we start to put more electrodes and sensors on them – and you can certainly access different regions of the brain through different blood vessels. But we thought this was the best starting point.

Synchron
On how patients learn to use the implant
For our first patient, we didn't really know what the signals would be like. So we got him to perform all these different tasks; try to move your left hand, right hand, left leg, right. We tried to figure out which ones were the best for us to use.
Over time, we've realized it's generally better for us to put the implant in, and say, 'here's the screen, try and make a click.' There's a little bar on the side that tells them how close they are to getting it, and they seem to work it out a lot quicker and better without us dictating exactly how they use it. It's often very hard for them to tell us exactly what's working, but once it's working, we'll keep using it, and that signal becomes stronger and more differentiated from the background noise, so the system keeps improving.
Translating Brain Signals
With the first patient, training took about 42 days, because we were doing all sorts of assessments and evaluations, and we weren't really sure what these neural signals would look like. The second patient, I think, took about seven days. And I believe every patient since then has got it working the day they've turned it on. They can use it almost immediately.
And it really doesn't need to be re-calibrated down the track, because we record local field potentials, which is sort of a large group of synchronized neural signals. If you're recording single cell activities with penetrating electrodes, for example, the brain moves a little bit. The cells move a little bit. What you were recording yesterday, or even this morning, might not be the same as what you're recording now. So constant calibration is required for some of those systems; not for ours.
On progress with human trials and the path to commercialization
We've completed an Australian human trial, on four patients with motor neuron disease (MND). None of those patients had serious adverse events, and they're all able to control a computer with their minds using the system. We then went to the US and started an early feasibility trial with six patients. So we'll combine those 10 to finish off the early feasibility study. Success on that will lead into a pivotal trial with the FDA, and success on the pivotal trial will give us a product that's deemed safe and effective, and ready for commercial release. Then doctors will be allowed to prescribe it, and it can be used by the community.
We're negotiating what the pivotal trial looks like with the FDA, enough to get sufficient evidence that it's safe and functional. The caveat is that it takes a long time to do these trials. There's obviously a period of running the trial, and there'll be a period of follow-up after the trial's finished. I don't like putting a date on when it'll be available, because we're not in full control of that process. But I'd love to see it complete in four or five years.

Synchron
On what it's doing for patients so far, and what it could do in the future
A simple, reliable approach is what we're going for. The patients we're speaking to right now aren't thinking about controlling super-sophisticated technologies. They want to be able to use a phone, communicate with friends, family, their carers and their loved ones. They want some independence. They're wondering if there's ways they can get back into the workforce, using word processors and whatnot.
Once they can do that, then for those that are interested, there's other future applications where we might be able to control a wheelchair, or even more sophisticated robotic arms and limbs. But let's get the first bit done, and make sure it's safe, and functional, and usable, and reliable.
The pathway for us is to get approval first for communication, and get that out there. While that's going ahead, we're having more discussions with the FDA on what safety measures they'd need, and how we can prove it's safe to use these devices to control something like a wheelchair, which obviously comes with its own complexities and risks, both to the patient and to others. We're in early discussions around that. But wheelchairs only have five or six controls, there's no reason why we can't provide the inputs to control a wheelchair.
For the patients, a lot of it's just about feeling human again. I was around at one of the gentlemen's houses the other day. He can't talk, but he's got the Stentrode implanted, so I can pull out WhatsApp and start communicating with him.
And what do we talk about? Well, he was giving me shit about the Tigers, how rubbish my football team is! Now it's been a few weeks, so I've got a few things to say back to him now! But it's just having conversations like that, connecting and having a laugh with people. Turning off the TV when you decide your kids have had enough. Telling your carer when you're in pain. Things that might not be necessary for human survival, but they make people feel alive and able to participate.
On whether Synchron's Stentrode could be used for human augmentation as well as medical uses
Anything that can be controlled with a computer can be controlled with this. Every time I give a talk at a conference, there's a gamer somewhere in the room asking if they can get one to be faster or better at their games, or to have access to more buttons or whatever. And yes, it's almost instant, you think about doing something and it comes up.
But we're really focused on the medical side right now, we're not looking at human augmentation. That's outside our wheelhouse, we can leave that to other cowboys. We want to help society in the best way we can. But there are plenty of medical technologies – take plastic surgery, which was developed for burns; now there's probably more plastic surgery for people who don't medically need it than for those that do. So it could creep out into that space.
The initial implants are more or less read-only. It's possible also to put electricity back in, and there's medical reasons why you'd want to do that. Medtronic, for example, puts stimulating electrodes all the way down through the brain, right into the middle of the brain, and they can send sort of bulk electrical pulses in there to stop people having Parkinson's tremors, or epileptic seizures, or certain depressive symptoms. So you can send signals into the brain to that extent. But will it get to the Matrix stage where you can download kung fu, or how to fly a helicopter? It doesn't look like it at the moment, but who knows!
Even when it comes to the visual cortex, I worked on the bionic eye project here. You need a lot of phosphenes, or pixels, essentially, to get a good image. And each electrode is one pixel. So you can imagine, you might be able to see letters reasonably easily with maybe 20, 30 pixels. But if you want to see a face, you're getting up around the tens of thousands before you're really seeing details. It's not outside the realms of possibility, but that's another level of technical development. I think the field is heading in that direction, and there'll be devices for a whole range of different applications, which is great.

Adam Glanzman/Synchron
On Neuralink and other competing companies
For anyone that works in this space, I think the attention that Elon Musk and Neuralink are bringing to this kind of work is fantastic. There's plenty of people in desperate need of this technology, and there's room for more than one player. If someone else can get there before us, and patients are better off? Great! We don't think that's gonna happen. We've found a way to make it safer and we're currently leading the way, but we're motivated by helping these people out, and so we want to support whoever we can to do that.
There's a couple of groups in the US that are doing the penetrating electrode arrays. Because of the invasive nature, my understanding is that they've been given FDA approval to implant it for a short period of time, but it needs to be removed. Now, you obviously can't force someone to have a surgery, so it's sort of a gray area telling people they need to have them removed.
Where Neuralink's concerned, there's no peer-reviewed research or detailed information coming out of that company, just what pops up on Twitter. So we know they've received some kind of FDA approval for human trials, but that's very vague, there's a lot of different conditional approvals the FDA might give. So we really don't know how far along some of these groups are.
There are some people we've worked with in the past, who were paralyzed, who went through trials using a device with a brain-penetrating electrode array. They could never use it at home, they'd go into the lab and use it, and they'd feel reconnected a little bit. And then it had to come out and then they felt like they were back where they started again. That can be devastating.
Ours never has to be removed, it's designed to be a permanent implant. Even in the cardiac world, if they've got a stent in a vessel and that vessel becomes re-blocked, they just put another stent in and leave the old one there. It's safer to leave one in there than try to remove it. We'll follow the same pathway.
On being recognized as a finalist at the 2023 European Inventor Awards
We've just been named as a finalist for a European Patent Office award for our technology. Awards like this, for us, are a way we can thank the people that have been involved in the journey. Our staff, our collaborators, and more importantly, the patients and their families who have thrown their hat into the ring to join our trials without any certainty that it'd be safe or functional. Thankfully, it's been both, but they took a big risk in putting their faith in us.
We thank Synchron's Nicholas Opie for his time and assistance on this story.
Source: Synchron
"interface" - Google News
June 27, 2023 at 09:47AM
https://ift.tt/nYZtp4c
Clever Aussie brain-computer interface leaves your skull intact - New Atlas
"interface" - Google News
https://ift.tt/WJTVHp5
https://ift.tt/jXrke3o
Bagikan Berita Ini














0 Response to "Clever Aussie brain-computer interface leaves your skull intact - New Atlas"
Post a Comment